On Thursday 11 October, when we were unexpectedly told that as a result of the CT scan and other tests, I needed to be re-admitted to hospital. That afternoon, the Interventional Radiologist, Dr. Patatas inserted needles through the right side of my back and extracted all the bile accumulation pressing on the chest as well as the liver, pancreas and the gallbladder. This procedure was done while I was under sedation so, I was mostly awake and very aware of what they were doing to me because at best it was uncomfortable and at worst, very painful.
After over two hours of ‘search and drain’ I was sent back to my room. Soon after, Dr. Patatas came to explain what he had done. Firstly, he had drained a huge amount of fluid, including over 1.5 litre of fluid which lodged itself between my right lung and the lining of the lung, plus another pool of bile just below that. He then implanted a drainage system which first emptied what was there, then had three tubes coming out of my back into collection bags to clear further accumulation as it formed. The bad news was that, even with the finest instruments they had, he was unable to locate the source of the leakage problem. So, the overall outcome of the procedure was successful by preventing things from getting worse; but the ability to fix the source of the problem remained undetermined.
Needless to say, Claire and I were less than happy with the overall picture that was emerging and began to reflect.
Fighting the First Battle seemed textbook-like; or as it was explained to us from the outset. As we started discussing this new challenge with the experts, certainty and clarity were not quite as evident as they previously were. The tone and language changed: ‘we have a number of options’, ‘we need to do more tests’, ‘another scan is necessary’, ‘let’s wait for a couple of days and see’. I was even given pep-talk by Dr. Petrou about holding strong, believing, resolve, etc. Traits he asked me to employ instead of his usual certain vision of what needed to be done next. What he was certain of however, the solution would not be a surgical operation; as any surgery carried a higher risk than other alternatives.
You don’t need to be a genius to frame the question: if you have a leak inside your body and surgery is not the answer, then what is? The answer is easy: you perform a ‘Procedure’. A cute and less threatening word than surgery; like saying to your unwanted employee: Joe, we are not ‘firing’ you, we are ‘letting’ you go!
A procedure in my case is getting access to my cavity through the creation of carefully plotted tracks, by inserting long needles guided by multiple scan images that reach the desired areas with microscopic instruments. As you can imagine, the human body is complex and variable in the ways it can be accessed and treated. ‘Surgery’ is a general and wide term that covers dozens of different techniques from incision to closing up. ‘Procedure, on the other hand employs less invasive techniques to deal with multiple ailments. For example, if you are unfortunate enough to need a biopsy, they perform a procedure to get tiny bits of the specific organ they want to test and analyse. Although it is not as dramatic or invasive as a surgery, such a procedure is performed at best under sedation, not general anesthetics, and it hurts like HELL!
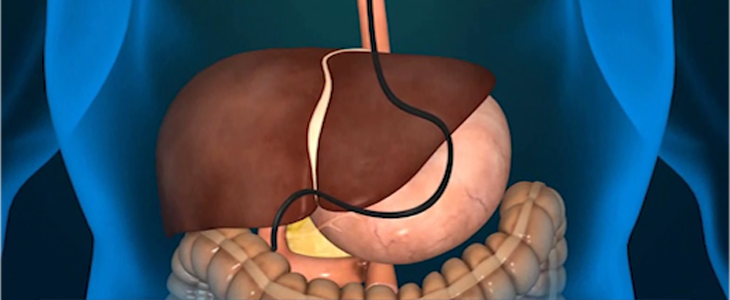
In my case, all procedures I was subjected to were all related to my biliary and liver issues. Let us classify all these procedures under a general term known as: ‘Endoscopic Retrograde Cholangio-Pancreatography’; or the more manageable acronym of ERCP.
On Friday 12 October, my brother Samir arrived from Amman, for moral and practical support. One of the first things he agreed with Claire was to give her morning break on Sunday 14 October, as it was her birthday. Not much of a birthday celebration but, it was better than nothing. Samir volunteered to drive early that morning to keep me company.
Soon after Samir arrived at the hospital, I suddenly became very unwell. I felt very weak and asked Samir to help me lie down on the sofa. I drew a sheet over me and began to dose off. I felt very cold and asked Samir to bring me a blanket, and then another. I then experienced violent spasms for what seemed like a long, long time. I was shivering from head to toe. What Samir thought was happening to me only he can say however, I truly thought I was going to shake myself into a thousand pieces. I told Samir that my ‘number was up’, which I have since learned scared sense out of him and all he could do to mask his own increasing concern was to say: ‘don’t be silly, today is Sunday and they don’t issue tickets’! Towards the end of this 25-minute horror episode, the ‘Birthday Girl’ arrived and she froze when she saw me, realising that I was very ill.
After multiple alerts to the medical staff, Dr. Neophitis, one of the surgeons involved in my case, turned up with a nurse pushing a trolley with various instruments of torture and at least 6 bags of one-litre saline solution. He asked Samir and Claire to leave the room, then explained he was going to push lots of fluid through my system as they suspected I had contracted an infection from fluid that had re-accumulated in my abdomen. A new word was added to our increasing vocabular – ASCITES. I was made to lie on my left side and using the drainage system previously installed by Dr. Patatas, he literally pumped the entire saline solution he brought with him into my cavity, causing a great deal of discomfort in the process. In return, he probably recovered a third of the now badly infected fluid, leaving me with surplus fluid I neither needed, nor asked for. I had developed Sepsis, although nobody actually told me the name of the infection at the time. It’s probably no exaggeration to say that Dr. Neophitis’ swift action saved my life that day.
The next day, enter Dr. Ioannou, a nephrologist, who explained the above and said the ascites was caused by lack of protein and the imbalance of my ‘albumin’, a protein produced by the liver to direct fluids through the bloodstream and on to your kidneys / bladder, instead of anywhere else such as the body tissues. In fact, albumin is highly concentrated in egg whites so, he recommended I consumed a lot of this mucus-like substance in any form from the humble boiled eggs, to yoke-free omelettes. I occasionally have boiled eggs, and less occasionally have an omelette but, I am no big fan of either. Claire however, took the task in hand and resolved to buy every Cypriot hen’s output of eggs, to help improve my albumin levels. For once, she and I were 180 degrees apart on such matters. The more she urged me to eat ‘this lovely boiled egg’ she held in her hand, the more determined I was not to do so. The confrontation between us reminded me of the classic Paul Newman movie: Cool Hand Luke, where he bet his fellow prisoners that he could eat 50 boiled eggs in a single sitting. His albumin must have shot off the charts!
Dr. Ioannou put me on large intravenous doses of albumin to replace what I had lost somehow. After the first day, my weight dropped by 1.5kg, but I still looked like a pear. The second day, I lost 2.7kg. The third day, I lost over 9kg. Dr. Ioannou demanded a re-weigh because he thought that last reading must have been wrong. He was right; it was wrong. When I stood on the scales in front of him, I actually had lost over 10kg in a single day!
That day, Dr. Petrou and team decided to perform the second procedure, to be carried out by Dr. Patatas and another interventional radiologist, Dr. Constantinou, to go through the drainage system, with the intention of applying a stent to the source of the leak. This procedure took place the following afternoon under sedation and again took over 2 and a half hours, resulting in failure to locate and close the source. I was returned to the ICU for a couple of nights, to combat the Sepsis and for the doctors to focus on my kidney function, which was giving them cause for alarm.
A further disappointment all round. However, everyone, including me, put a brave face on things, repeating phrases like ‘we fight on’, ‘let’s keep positive’ and so on.
On 18 October, Dr. Petrou came and declared that they developed a new strategy: the next procedure would employ a second specialist team that would get access to the leak area via the mouth, through the stomach, the common bile duct and into the troublesome region. It was on that day that I officially met ‘ERCP’ when Dr. Patatas explained what was going to happen. The first team, led by Dr. Patatas, would go through the previous route to meet the second team in a battle tactic known to medical people by the cutely named ‘rendezvous technique’. Dr. Petrou seemed upbeat and enthusiastic, so much so, he drew for us a diagram explaining the battle field and how the rendezvous technique would work.
The whole procedure looked impressive and we said: ‘well, let’s do it then’. Dr. Petrou poured cold water on our enthusiasm by declaring it cannot be done until next Monday 22 October because not all the ERCP experts were available yet, blah, blah.
18 October was ‘good news/bad news’ and marked one of my lowest points of the entire experience to date. Claire had to pull out all the stops to get me to resurface from my gloom.
Monday 22 October took a million years to arrive. My spirits were gradually lifting, and I was ready to go to battle in my limited contribution to the process beyond turning up.
The other small item of cheer was the anaesthetist promised I would be under general anaesthetic and would feel nothing. The rendezvous procedure was to start at around 14:00 and when the time finally arrived, I was kissed and waved goodbye by Claire, then wheeled out to the operating room, full of hope.
Three hours later I was brought back to my room and on the way, I could hear a faint and unclear conversation going on between Claire and Dr. Patatas. Even in my highly drugged state and being 90% asleep, I gathered enough negative words and vibes to lead me to conclude the rendezvous technique procedure had failed.
Claire spoke to me and asked me how I felt. I said I was very cold so, she and the duty nurse piled blankets over me until I could regain control of my jaw to form some meaningful words. My question to Claire was: it failed, didn’t it? She said it did and somehow or another I managed enough control of my chattering jaw to form a fully understandable semi-sentence, which I repeated over and over again: ‘That fucking useless Dr. Patatas!’ Poor man, he was part of a sizeable team and I have no idea why I particularly picked on him. As I slowly came round, yet again, Claire had to draw on all her energies to remind me of the need to remain positive and optimistic. Eventually, I pulled myself together and tried to look forward to the next day.
So, the Second Battle was in full swing and the cancer demons seemed to be winning 3/0 so far.
The following day, Dr. Petrou came in looking less than his usual debonair and confident self to confirm what we already deduced. The medical team were now scratching their heads for a way forward. Dr. Petrou even admitted he had never come across such a case but, he was determined to find a solution. Nice to see a medical professional determined to find a solution to a medical puzzle but, not at the possible expense of my own health! He said that he would be seeking advice amongst his network of experts but in the meantime, they would continue to stabilize me and even improve my various vitals, as well as introducing ‘Contra-lock’ medication to heal my stomach which was damaged as a consequence of the gastric invasion by the second half of the rendezvous team. That damage essentially turned off my entire appetite, even for water and I was physically unable to ingest anything at all.
I remember thinking one night: ‘every time I find myself at a new low point, instead of feeling sorry for myself, maybe I should remember that it must be possible to descend further down the abyss so, let’s be thankful for where I stand’. I must confess that I counter-argued my own logic by replying: ‘yeh right, just like anyone should be thankful that they only lost one arm in an accident where it might have been two!’ So, I went to sleep that night of Tuesday 23 October feeling extremely sorry for myself. I will return to that hellish night in a later blog because it marked the lowest point of my entire experience to date.
On Wednesday 24 October Dr. Petrou visited again and said he had a new plan but, it would require a great deal of preparation, including the use of very fine paediatric instruments in order to perform a more intricate maneuver to locate and stem the leak. However, he needed to order such instruments which were not readily available. He also needed to book a highly specialized gastroenterologist to lead a new second team to repeat the rendezvous technique. In short, there was little prospect of this procedure taking place before the following Monday 29 October. You guessed it, another new low was reached. Almost as an afterthought, Dr. Petrou added that an MRI (not CT) scan would be needed to map my ‘biliary tree’; a network of fine vessels that connects the liver, pancreas and gallbladder. He said this would be arranged as soon as possible.
That MRI was not arranged for that day, or Thursday, or Friday, meaning it was now highly unlikely to take place before Monday morning 29 October, the nominated day for the procedure. Claire and I came to the conclusion that our angelic doctor was buying himself some time from our depleting stock of patience!
On Tuesday 30 October, Dr. Petrou suddenly burst into the room around 12:30, accompanied by a casually dressed gentleman and with great deal of pride and flourish, introduced him as: Dr. Ioannis Kaimakliotis; a specialist in difficult situations such as mine. Dr. K took over the lead and began to explain what and how he was going to perform this highly delicate ERCP procedure. Amongst his non-stop and flowing questions and explanations, we managed to ask a few questions of our own, which he answered. Dr. K declared himself to be ready to ‘go in’ the following day, 31 October 2018; Exactly two full months after the main operation to remove the tumour was performed by Dr. Petrou and team. It seemed to me like two years.
Was that going to be the end of the Second Battle?
Not quite. On Wednesday, I was yet again wheeled to an operating room, stripped naked, made to lie on my stomach and heavily sedated by Dr. K’s own anesthetist. Some 90 minutes later, I found myself back in my room with Claire waiting for an explanation. Dr. Patatas came and explained the new combination team had made progress. Dr. K managed to go in, identify two, not one problem sources. He used very complex techniques to insert mesh tubing to make it possible, at a later date, for his and Dr. Patatas’ teams to re-enact the ‘rendezvous technique’ and put in place a more permanent solution to the leak.
So, we made progress and gained ground on the demons but, we did not defeat them completely; not yet anyway.
I was released on Saturday 3 November to wait for the call from Dr. Patatas to say everything was ready to perform Procedure number Six which would be the penultimate procedure to finally stem the leak. He said the call would likely be week beginning 12 November. I was happy to do that as I looked forward to home time, especially where we had Faye and boyfriend Adam, and my niece Mais and her husband Muhammad, all loveable and delightful company.
The call actually came on Monday 5November; a full week early, asking us to return to hospital the following morning to prepare for Procedure no. Six.
On Tuesday, after some delay, D. Patatas and Dr. K were waiting for me in the theater; they both seemed confident and optimistic. They were justified in assuming that attitude because the work required to prepare for the final solution, which is to connect the two severed ends of one of the biliary ducts with a six-centimeter metal stent that would house and support the proper stent to be inserted in the seventh and final procedure.
Dr. Patatas wanted to keep me in hospital until things were stable and ready for the final procedure but by that time, I felt I had enough of the American Medical Center, of being hospitalized, deprived of sleep and I resolved to challenge his decision. The showdown with Dr. Patatas came on Thursday 15 and I put my foot down. Finally, he relented and said I could go home but, I had to go to a local clinic and provide blood samples, take antibiotics, and other medications to prevent any possible infection before the final procedure. I was happy to agree to anything that let me out of that place for a brief respite.
That weekend, Leila, Rosy and my nephew Khalil visited lots of home cooking and sharing a huge order of take-away curry with the Eftekhars.
On Monday afternoon 19 November, Claire drove me to Nicosia to be prepared for the following day’s procedure, including nil-by-mouth from midnight, etc.
The procedure took place late afternoon on 20November where I was put under strong enough sedation to feel nothing. However, I was quick to come round when Dr. K and Dr. Patatas finished their business and disappeared somewhere. The theater nurse was the only person I could ask the question; Did it work? Her answer was absolute music to my ears: yes, the procedure was successful. The other piece of good news was that Dr. Patatas had removed the last drainage tube and stitched the wound, hopefully for the last time.
I was reunited with Claire in my hospital room and she had already gathered the news elsewhere so, we had a private emotional moment I will never forget.
Two days later on Thursday 22 November, I was released with prescription for a double antibiotic course for 7 days to fight off any possible bacterial infection as a result of the last procedure. Dr. Patatas still wanted me to have regular blood tests sent to him to monitor my recovery progress.
And so, after 44 days of struggling with so many ups and downs of 7 procedures, we felt that although we lost a few rounds, we have actually won the Second Battle against cancer! We realise that there is at least one more battle to go through the oncology process of finding out whether or not cancer is still lurking somewhere in my body. That in itself will signal more battles ahead. Even if the oncology examination finds no traces of cancer, we already learned that I would need regular tests and scans for at least the next five years. However, we cannot live our lives in constant fear; we must move on as best we can; taking each day as it comes.
Although the last procedure was not the absolute end of the Second Battle, what came afterwards was not of sufficient significance to recall in this blog.
I am almost done with the “Fighting Cancer” series of blogs; just two more postings to round things off and then that will be that.
Thank you for continuing to read my blog and the occasional sending comments of support and encouragement.
If you wish to continue to read the rest of this series of blogs but had not subscribed, please do so at the very bottom of this blog page. You may unsubscribe at any time you like.
Thank you.


